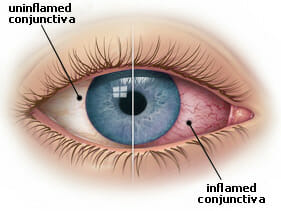
Conjunctivitis
Conjunctivitis, commonly called pink eye, is an inflammation of the conjunctiva, the thin, clear tissue that cover the white part of your eye.
- Symptoms
Patients typically have an eye that appears read and irritated. It is often accompanied by a discharge (clear, yellow, or white), itching and a feeling like something is in your eye. Occasionally blurry vision may occur. - Causes
Pink eye may be caused by a viral infection, bacteria or allergic reaction. The viral and bacterial pink eye are highly contagious. - Prevention and Treatment
If you are experiencing any of these symptoms you should contact your eye doctor right away. To avoid spreading conjunctivitis wash your hands often and don’t touch the infected area with your hands. You also don’t want to share wash cloths or towels. Avoid using makeup which may become contaminated. Sometimes your eye doctor will need to prescribe antibiotic eye drops and ointments to treat the conjunctivitis.
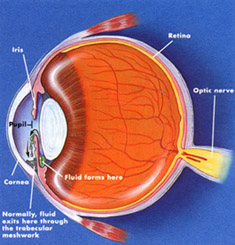
Glaucoma
Glaucoma is a very common eye disorder affecting millions of Americans. It is typically caused by too much pressure on the inside of the eye. Fluid in your eyes helps to nourish and cleanse the inside of your eyes by constantly flowing in and out. When too much fluid is made or if the fluid is prevented from flowing out, the intraocular pressure builds and has the potential to damage the optic nerve. This leads to a gradual loss in peripheral vision.
- Symptoms
Those suffering from open-angle glaucoma experience a type of tunnel vision; their field of vision gradually decreases from the outer edges of vision towards their central vision. It can eventually lead to blindness. The loss of vision is a slow progressing process and most patients with glaucoma will not notice any symptoms. Narrow-angle glaucoma, which is rare, carries symptoms of sharp pain in the eyes, blurred vision, dilated pupils, and even nausea or vomiting. It can cause blindness in a matter of days, and requires immediate medical attention. - Risk Factors
Heredity seems to be a risk factor. Also, you may be at greater risk if you are over 45, of African descent, near-sighted, or diabetic. Finally, if you have used steroids for a long period of time, or if you have suffered an eye injury in the past, you have a greater chance of developing glaucoma. - Prevention and Treatment
Early diagnosis and early treatment are the key with glaucoma. Patients with glaucoma and patients who are at higher risk for glaucoma should have their eye pressure and their peripheral vision checked regularly. There is no way to prevent the glaucoma from occurring, but typically the use of medication eye drops is enough to stop the progression of the disease. In some cases surgery may be necessary. - More Information
Glaucoma Research Foundation: http://www.glaucoma.org
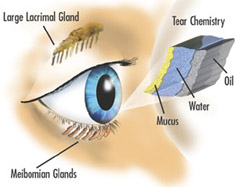
Dry Eye Syndrome
Dry Eyes affect almost 10 million Americans. Dry Eye Syndrome can be caused by a lack of tears or in some cases there are ample tears, but they have poor quality. Tears lubricate the outer layer of the eye, called the cornea. If there are not enough tears or if the tears are not composed of a proper balance of mucous, water, and oil, the eye becomes irritated.
- Symptoms
Dry Eye Syndrome leads to a number of symptoms: itching, irritation, burning, excessive tearing, redness, blurred vision that improves with blinking, and discomfort after long periods of watching television, using a computer, or reading. - Risk Factors
There are many factors that can contribute to Dry Eye Syndrome. These include dry, hot, or windy climates, high altitudes, air-conditioned rooms, and cigarette smoke. Contact lens wearers, people with drier skin, and the elderly are more likely to develop Dry Eye Syndrome. You may also be more at risk if you take certain medications, have a thyroid condition, a vitamin-A deficiency, Parkinson’s or Sjorgen’s disease, or if you are a woman going through menopause. - Prevention and Treatment
There are many options for the treatment of Dry Eye Syndrome. In some cases, simply the use of lubricating eye drops is enough to improve the situation. In more severe cases, medication eye drops, oral supplements or even surgical correction are better options. - More Information
Complete Family Eyecare Dry Eye Center of Excellence: Dry Eye Center of Excellence
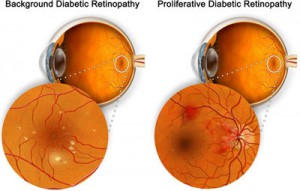
Diabetic Eye Disease
Diabetic Eye Disease is a group of eye problems that can occur in patients with diabetes. Diabetes can affect many part of the eye, most notably the lens and the retina. Patients with diabetes are two times more likely to develop glaucoma. High levels of blood sugar and fluctuating blood sugar over time will damage tiny blood vessels in your eye and make them leak. New vessels may form to replace the damaged vessels, but the new vessels tend to be weaker. This combination of poorly functioning blood vessels leads to starvation of the retina, which overtime causes vision loss.
- Symptoms
Often there are no symptoms early on when a patient is experiencing Diabetic Eye Disease, that is why it is so important that any person with diabetes has an eye exam a least every year. Some symptoms a patient might experience are:- “Floaters” – small specks that pass across your field of vision, made up of cells floating in the transparent gel of your eyeball
- Difficulty reading or seeing things close-up
- Sudden loss of vision
- Flashes
- Blurred or darkened vision
- Risk Factors and Treatment
If you have diabetes, make sure you regularly see your family doctor and work to control your blood sugar level. This will reduce your risk of getting diabetic retinopathy. If you are experiencing some of the symptoms listed above, you should call your eye doctor right away. Many treatment options are available.
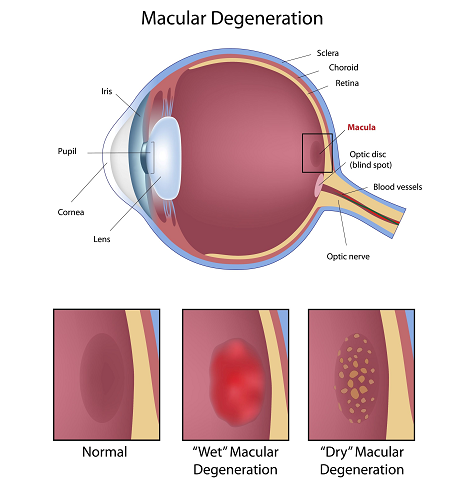
Macular Degeneration
Macular degeneration is the leading cause of blindness in Americans over the age of 65. It is a disease that affects the small, central area of the retina responsible for precise central vision, known as the macula. The macula allows us to see the fine detail of whatever is directly in front of us. Macular degeneration occurs when the macula begins to deteriorate; this leads to loss of central vision.
- “Wet” vs. “Dry”
Macular degeneration has two forms: dry (not involving the formation of new blood vessels) and wet (includes the formation of new blood vessels). Most often, macular degeneration is accompanied by the formation of yellow deposits called “drusen” under the macula. Wet macular degeneration accounts for about 10 percent of cases – this type is typically associated with more severe vision loss. - Risk Factors
A number of uncontrollable factors contribute to macular degeneration, including genetics, age, sex, eye color, farsightedness, and race. Risk factors you can control include smoking, high blood pressure, obesity, exposure to harmful sunlight, and diet. - Symptoms
It is difficult to detect dry macular degeneration in the early stages and the onset is typically gradual. The most common symptoms, when detected, include a spot of blurry vision, dark vision, or fuzzy and distorted vision. Often macular degeneration is detected by your eye doctor before symptoms even begin to occur. - Prevention and Treatment
While there is no cure for macular degeneration many treatment options are available to slow the progression of the disease. Many patients are put on nutritional supplements by their doctor. Prescription medications and laser treatments are also available and should be discussed with your eye doctor.
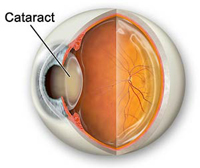
Cataracts
Cataracts are a cloudiness that occurs in the lens of the eye. The lens is made mostly of water and protein arranged to let light through. Sometimes the protein clumps, blocking light and making the lens appear cloudy. A clear lens is necessary for crisp vision, as this lens get cloudy and vision will begin to blur.
- Symptoms
A person with cataracts may encounter faded colors, problems with light (such as glare, halos, or headlights that seem too bright), poor night vision, double vision, or multiple vision. - Prevention and Treatment
Your eye doctor can detect the presence of cataracts through a thorough eye exam, including a visual acuity test and dilation of the pupils. Treatment is available to prevent cataracts and decrease symptoms. Once a cataract progresses to a level where it interferes with your daily activities, it can be surgically removed. This is a decision you should discuss with your eye doctor.
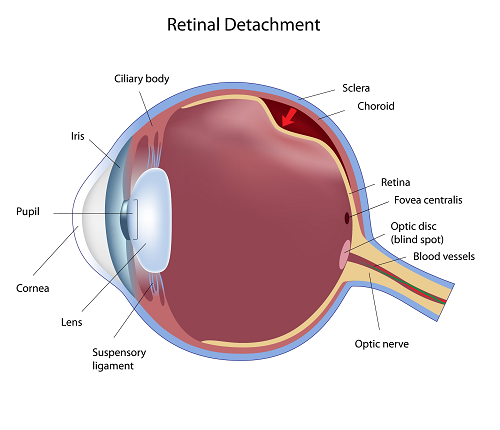
Retinal Detachment
The retina is the part of the eye which collects light and transmits the light messages to the optic nerve and brain; it lines the inner back wall of the eye. When the retina separates from the back wall, it is known as retinal detachment. It is a serious condition which can cause permanent damage and vision loss if not treated quickly.
- Symptoms
Patients with a retinal detachment may experience a variety of symptoms: Floaters, which look like small particles or fine threads or bugs in your vision, Flashes of light may be noticed; a curtain or cobweb type shadow in your vision. Some patients experience “wavy” vision or blurred vision. Anyone who experiences new floaters or a change in their floaters, flashing lights, a curtain or cobweb type shadow in their vision or a total loss of vision should see an eye doctor as soon as possible. - Risk Factors
Eye injuries, tumors, and cataract surgery can cause retinal detachment. Near-sighted individuals and the elderly are at greater risk for spontaneous detachment. Also, diabetic retinopathy, a condition associated with diabetes, can cause bleeding which leads to retinal detachment. - Prevention and Treatment
The best chance for recovery comes with immediate care from your eye doctor. A variety of treatment options are available typically involving surgery.
